Calling an ambulance for a hangover and turning up at A&E with a broken nail - these are just some examples of the time-wasters Cumbrian health staff have had to deal with in recent months.
Medics are speaking out as the already overstretched local NHS lurches towards winter, with predictions that 999 services and emergency departments will be pushed to the brink.
Leaders say that they are putting in place detailed plans to help ease the pressures, but they need the public to help too.
They are urging people to think before calling an ambulance or heading to A&E, and only use these in genuine emergencies.
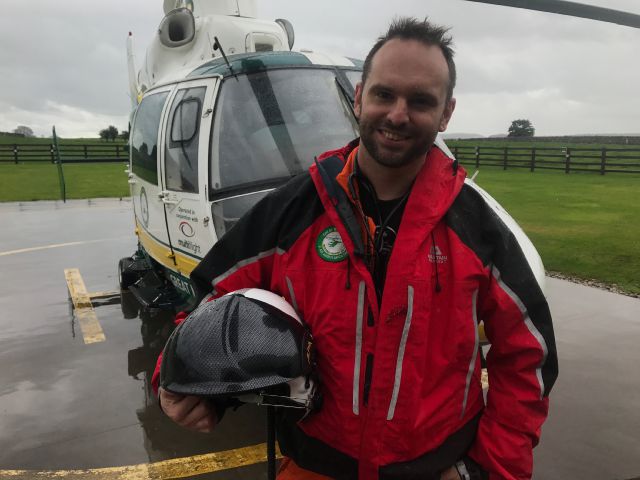
Vinny Romano is an advanced paramedic covering Cumbria. He says calls are increasing year on year, and winter is their busiest time.
The rise in demand is largely due to an increase in trips, slips and falls in colder weather and existing health problems being exacerbated in colder weather, particularly among the elderly and infirm.
There is also a rise in people going out over the Christmas and New Year period, meaning more call outs at weekends.
Meanwhile, hospitals are also under pressure, with already busy A&E departments in Carlisle, Barrow and Whitehaven seeing the numbers coming through their doors soar for the same reasons.
High-profile shortages in social care mean that patients can't always be discharged quickly from hospital, resulting in bed-blocking.
This again has a knock-on effect for the front of the hospital, making it difficult to admit those who are waiting for beds.
But although there are wider problems to address, including funding, staffing and patient flow, both ambulance and A&E staff say that the patients themselves have a big role to play.
Mr Romano said that the number of non emergency calls they deal with is getting higher.
“About 80 per cent is what we would call ‘low acuity’. It’s higher than it ever has been," he said.
He gave an extreme example of some of the people who waste their time when they could have sought help elsewhere.
“I was called to a 25-year-old not that long back who was feeling nauseous and dizzy after drinking until 2am. It’s quite easy to diagnose a hangover.
“I do not think they realise the implications it has. We are a finite resource.
"We are there when people need us and will do everything we can for that patient, but it means that ambulance isn’t there for another patient.
“If we are getting sent to patients that do not need to go to hospital, it’s a time-consuming process to assess them and refer them to where they should have gone in the first place."
Andy Knox, executive lead for health and wellbeing at Morecambe Bay Clinical Commissioning Group (CCG), said they recently had a woman with a broken nail turn up in A&E and have also seen young people coming in with hangovers after getting drunk on a night out.
There was also a woman who was already visiting a relative in hospital and thought it would be more convenient to go to A&E while she was there, rather than making a GP appointment.
“This costs us hundreds of thousands of pounds every year," he said.
“We are encouraging patients to use the NHS in the best way and to think about self care, walk in centres, GPs, out of hours GPs, nurse practitioners.
"Really, emergency departments are absolutely only for emergencies."
Dr Knox said A&E departments also see patients coming in because they haven’t registered with a GP.
“There’s no excuse for that," he added.
Mr Romano, who works for the North West Ambulance Service (NWAS), said there is also a myth that they will get seen more quickly if they go to hospital by ambulance.
“You do see messages on social media and people saying ‘call an ambulance, you’ll get seen quicker’," he said.
“They think they will jump the queue. That’s not accurate, but that’s what they think.
"In fact they will be triaged like everyone else and the person who needs to be seen first, will be.
He added: “The message is really about choosing well. We are always going to capture some low acuity, but we get people calling for so many things that aren’t emergencies.
“We get people calling who have hurt their fingers for example. They are more than capable of going to a walk-in centre."
Medics planning for winter
Hospitals across Cumbria have been finalising their plans so they are best placed to cope with the predicted surge in demand this winter.
Nationally, many are predicting the worst winter for the NHS - with already struggling A&E departments feeling the brunt of the pressure.
Although still not meeting Government waiting targets, emergency departments at both the North Cumbria and Morecambe Bay trusts are now regularly performing above the national average.
But with high-profile bed-blocking problems in the county's hospitals and shortages of social care in the community, the balance could easily tip if demand for emergency services rise as predicted.
That's why bosses are appealing to the public to make sure they only use A&E and ambulance services in genuine emergencies, and instead get advice from other services for non-urgent problems.
Paul Grout, deputy medical director and consultant for emergency medicine at University Hospitals of Morecambe bay NHS Foundation Trust, said that this year they are already under more pressure than others.
Dr Paul Grout
“Winter occurs every year so it doesn’t come as a complete surprise," he said.
"At the moment, this year and last year, it’s been unusual in that the summer period has not wound down like it normally does.
"This is true not just for our trust, but across the whole country.
“Usually the pressure goes off, then you get to winter and you get ready for an upsurge," he explained.
He said that it is not just the number of patients coming through the doors that increases workload, but that those who do tend to have more complicated illnesses, particularly elderly people.
Dr Grout said that the existing pressures and rise in demand is combined with other problems, such as high-profile shortages of nursing staff - meaning they are unable to simply open more beds.
“We’ve been proactive in going out and recruiting from abroad, but that takes time to go through the system," he said.
“We’ve also got problems because we have not cleared out in the same way as we usually would during the summer.
"There are a number of patients in the hospital that we are waiting to get into nursing and residential homes. So we are starting from not a good baseline, and that’s not unique to our area."
John Ferris John Ferris, clinical director for emergency and acute care at Carlisle's Cumberland Infirmary and Whitehaven's West Cumberland Hospital, said although waiting times are improving, they are still overstretched.
He said that if people used the right service for their needs, it would allow A&E staff to focus on the most poorly patients.
"We are going to be busy. Our emergency departments on both sites are busy regardless of whether it is summer or winter.
"The people we see at this time of year tend to be older, frailer patients with lots of medical conditions.
"The temperature and weather tend to play a part.
"If it is icy we get more falls and if the roads are slippy there will be more road traffic collisions," he explained.
"There is also a higher prevalence of infections and common colds.
"They spread through society more quickly and people can become hospitalised if they have complications.
"What we know is that year on year, we see an increase in the numbers of people attending emergency departments. We obviously have to be mindful of that increase in workload."
But Dr Grout said there are things they are doing to help ease the pressures. In his trust, this includes:
– Identifying patients with chronic respiratory problems and issuing rescue packages so they can get antibiotics or steroids early on, before they deteriorate and need admitted
– Referring patients to a short-stay ambulatory care unit, which allows them to be monitored and undergo tests without having to be admitted. Similar units are also used in north Cumbria.
– Ensuring ward rounds take place earlier in the day, so patients can get home earlier and free up beds for others.
– Establishing a team to help tackle bed-blocking. Based in the hospital, they are able to go out to a patient’s home and provide basic care and support while longer term care packages are put in place.
North Cumbria has been given some extra funding to tackle winter pressures, but Dr Ferris said the majority was not being spent in A&E.
In the past he said it has been a case of "fighting fires" through winter, but now they are looking at capacity in the wider system.
"There is a danger of thinking we are the only ones in this position, but we have to realise that this isn't just a problem that's unique to emergency departments. It is the whole health system.
"To be perfectly honest, a lot of the problems we experience here are a direct reflection on other people being very busy delivering their own service, so this is the right thing to do," he said.
That includes rolling out a successful pilot scheme from Eden in which therapy teams work with paramedics to assess patients, particularly elderly people who have had falls, in their own home and see if they can be kept out of hospital. This will be extended to Carlisle.
Dr Grout said many people feel their relatives should be in hospital, but it is not necessarily the best place as being in a bed, even for a few days, leads to loss of muscle and higher risk of falls or infection.
“You can end up with someone who was living independently when they came in but, by the time they are discharged their care needs are significantly greater. That’s one of the things we want the public to understand. The majority of times people are better off in their own homes, if they can be," he explained.
Dr Ferris said he is confident that they can cope with whatever winter throws at them, but urged people to think before turning up.
"A big thing for us will be making sure that when someone has got a problem, they go to the right place. That's about educating patients and linking closely with primary care services," he added.
Advanced paramedic, Vinny Romano, said they are also increasing their resources at peak times and recruiting extra staff, but patients can help to avoid the services becoming overwhelmed.
“Hospitals are also under more pressure, which has a knock on effect on us when we are waiting to hand over patients. That can delay us.
"I also think people think we are the one service they can call on and we will come. That’s how we are viewed. If in doubt, they phone 999.
“There is so much information out there they can access before they come to us.
"Bear in mind we are an emergency service, and that’s what we should be used for."
Who should you call if you feel unwell?
NHS 111 - This is a free phoneline which the public can call for non-urgent medical advice. If they think you should see a doctor, attend a walk-in centre or go to A&E, they can advise you accordingly.
Pharmacists - These are staffed by trained medical professionals who can provide health advice and over the counter treatments on a wide range of conditions. Again they can refer you elsewhere if necessary.
GPs - General health complaints that can't be dealt with by a pharmacist. Bear in mind many practices now use phone call assessments to decide whether or not a patient needs to be seen in the surgery.
Children - Parents and carers are advised to download the free 'NHS Child Health' app for advice on a wind range of health complaints.
Walk-in centres - There are several walk-in centres across the county for those with non-urgent injuries and health issues.
A&E - Only use this service for serious and life-threatening injuries and conditions.
Ambulance - Life-threatening emergencies only. Call 999 for chest pains, difficulty breathing, if someone is unconscious, if you think someone is having a stroke, for severe burns or severe bleeding.








Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules here